Duodenal Switch, also known as Biliopancreatic Diversion with Duodenal Switch (BPD/DS), is a restrictive and malabsorptive surgical intervention for obesity. It is known for its more significant weight reduction and resolution of comorbidities than other surgeries. DS/BPD and its cousin SADI-S are the most complex procedures compared to all other bariatric surgery options, leading to a higher risk of nutritional deficiencies.
The skill and experience of the bariatric surgeon are crucial factors for the safety of the patients and the outcome of the procedure.
Two Stages of DS Procedure
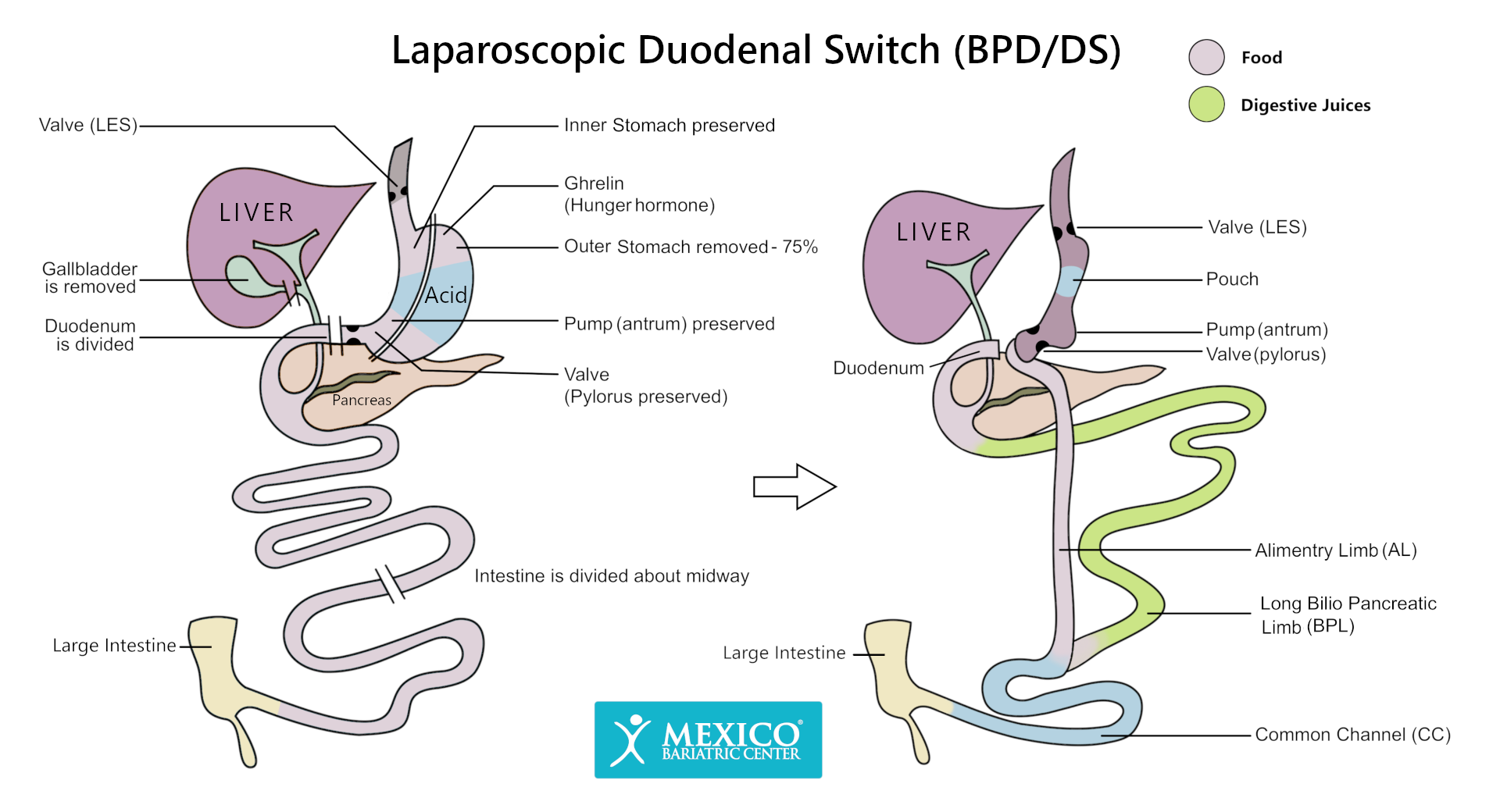
Stage 1 – Restrictive
In Stage 1 (Restrictive), nearly 70% of the stomach is removed at the greater curvature (also known as a vertical sleeve gastrectomy). The remaining portion of the stomach is fully functional in the shape of a banana, holding about 3-5 ounces, restricting the amount of food consumed. The pylorus valve will continue to control the stomach’s emptying process into the small intestine. Because of this, patients do not experience dumping syndrome like many other weight loss surgery patients who undergo RNY gastric bypass.
The upper portion of the duodenum is useful, as it helps food digest into a good consistency before going to the small intestine. This allows the body to better absorb nutrients and vitamins such as Calcium, Iron, and Protein when compared to gastric bypass surgery patients.
Many surgeons believe that removing a portion of the stomach significantly reduces the amount of ghrelin-producing tissue and acid in the stomach. Ghrelin is well known as the hunger hormone, and reducing the amount of the hormone in the body helps to reduce a patient’s appetite, leading to greater weight loss.
Over time, the stomach will stretch; nearly 9-12 months post-op, the stomach will double in size, and many patients will be able to consume about 60% of their intake before surgery. The restrictive part of the Duodenal Switch procedure is not reversible.
Stage 2 – Malabsorptive
The intestines are switched via the duodenal ileal anastomosis such that food from the stomach and the digestive juices travel on different paths and never mix until they meet at the end of the small intestine. The alimentary limb is responsible for carrying the food, while the biliopancreatic limb carries the bile and other digestive liquids.
The common channel or limb meets the small intestine, where it joins the large intestine. This is where the patient’s food, bile, and digestive liquids mix and where nutrients are absorbed into the body. Since the common channel makes up such a small section of the small intestine, fats, scratches, and complex carbohydrates are never fully absorbed, leading to weight loss.
Because of the malabsorption of fats, many fat-soluble vitamins such as A, D, E & K become low in the body, leading to deficiencies. All Duodenal Switch patients are required to take regular vitamin and mineral supplementation for their lifetime. The intestinal switch portion of Duodenal switch surgery is fully reversible.
Hess Method
Many surgeons will change the common channel length. They calculate this by taking the length of the alimentary limb and multiplying it by the small bowel length by 40%. The remaining 60% will carry the digestive juices through the biliopancreatic limb. The Hess Method, established in 1988, is best known for determining limb lengths and common channel length while thinking of the patient’s BMI, overall weight loss goals, age, and weight.
The Hess method uses 50% of small intestine length as a Biliopancreatic Loop (BPL), 40% as an Alimentary Loop (AL), and 10% as a Common Loop (CL). Not all surgeons use this method, but some do to achieve the best results for each patient.
Appendix/Gallbladder Removal
Many surgeons also suggest an appendix or gallbladder removal during the procedure. Some surgeons even require the gallbladder to be removed because of the 30% chance of developing gallstones after surgery and rapid weight loss. The appendix may be removed so that there is no future confusion regarding stomach issues and symptoms and whether they are a result of surgery or appendicitis.
Patient Success
In general, most BPD+DS recipients have incredible results and can lose up to 85% of excess weight loss in the first 12 months on average.

Patients who have had prior sleeve surgery and faced undesirable outcomes can get back on track by undergoing duodenal switch surgery revision.
Related:
